


If you’ve been diagnosed with obstructive sleep apnea (OSA) or think you might have the condition, you may have questions about how to treat it.
There are several treatment options; the most effective way to treat your sleep apnea depends on the severity of your condition.
Generally, mild to moderate cases can be effectively managed with the same techniques used to treat primary snoring (i.e. non-apnea). Severe cases where your AHI is over 30 are best managed with CPAP.
In extreme cases where CPAP is not tolerated and there is a clear physical obstruction, surgery can also be an option.
This article explores the various methods that can be used to manage obstructive sleep apnea.
Each category has links to other useful SnoreLab articles on the subject.
Side note: what determines sleep apnea severity?
The severity of sleep apnea is split into mild, moderate and severe. These designations are based on how many times you experience apnea or hypopnea episodes per hour – your AHI score. This is where your breathing completely stops or partially stops for 10 seconds or more.
Make sure to read our article about sleep apnea diagnosis to understand sleep studies, the AHI score and classifying the severity of obstructive sleep apnea.
If your sleep apnea is at the milder end of the spectrum, you can treat it by making some targeted lifestyle changes.
What is most effective depends greatly on what is responsible for your sleep apnea in the first place. Generally speaking, the following lifestyle changes have the most positive impact:
Your weight has a significant influence on your likelihood of developing obstructive sleep apnea. Simply put, the heavier you are, the more likely you are to suffer from OSA.
Side note: the statistics of weight loss and sleep apnea
Some epidemiological studies indicate that 70% of patients experiencing sleep apnea are obese, and 40% of obese people are suffering from sleep apnea [1].
Promisingly, research has demonstrated that losing 10-15% of your body weight can half the severity of your sleep apnea [2], and that losing 60% of body fat can eradicate sleep apnea for around 86% of obese people [3].
There’s no shortage of advice or special diets when it comes to losing weight. It can all be a bit confusing and overwhelming. No single technique works wonders for everyone, and drastic solutions are rarely stuck at for very long.
Instead, be sure to check out SnoreLab’s SMART strategy for effective, sustainable weight loss and also have a read of our full article of the impact of weight on snoring and sleep apnea.

Smokers, and even passive smokers are more at risk of snoring and experiencing sleep disordered breathing [4][5].
Some studies have found that smokers are 2.5 times more likely to suffer from obstructive sleep apnea [6].
Quitting smoking has shown to reduce your likelihood of experiencing sleep disordered breathing [7]. This is because smoking contributes to greater inflammation and irritation in the upper airway which predisposes it to vibration and collapse [8].
Further, a nightcap is also not ideal for healthy sleep. Alcohol causes your muscles to relax – even more than they do normally when you fall asleep. It therefore increases the collapsibility of your airway and heightens the risk of experiencing apneas.
SnoreLab users amongst many others have found that reducing their alcohol consumption yields drastic reductions in their snoring and sleep apnea.
.png)
More than half of all obstructive sleep apnea cases are referred to as “position-induced” sleep apnea [9], where the severity of the condition is made worse by back-sleeping.
By sleeping on your back, your mouth has a tendency to fall open. This changes the shape of your upper airway and makes obstruction more likely.
Sleep apnea can therefore be massively reduced by switching to side-sleeping. There are many techniques you can use to make this change – be sure to check out our guide to sleeping position and snoring.
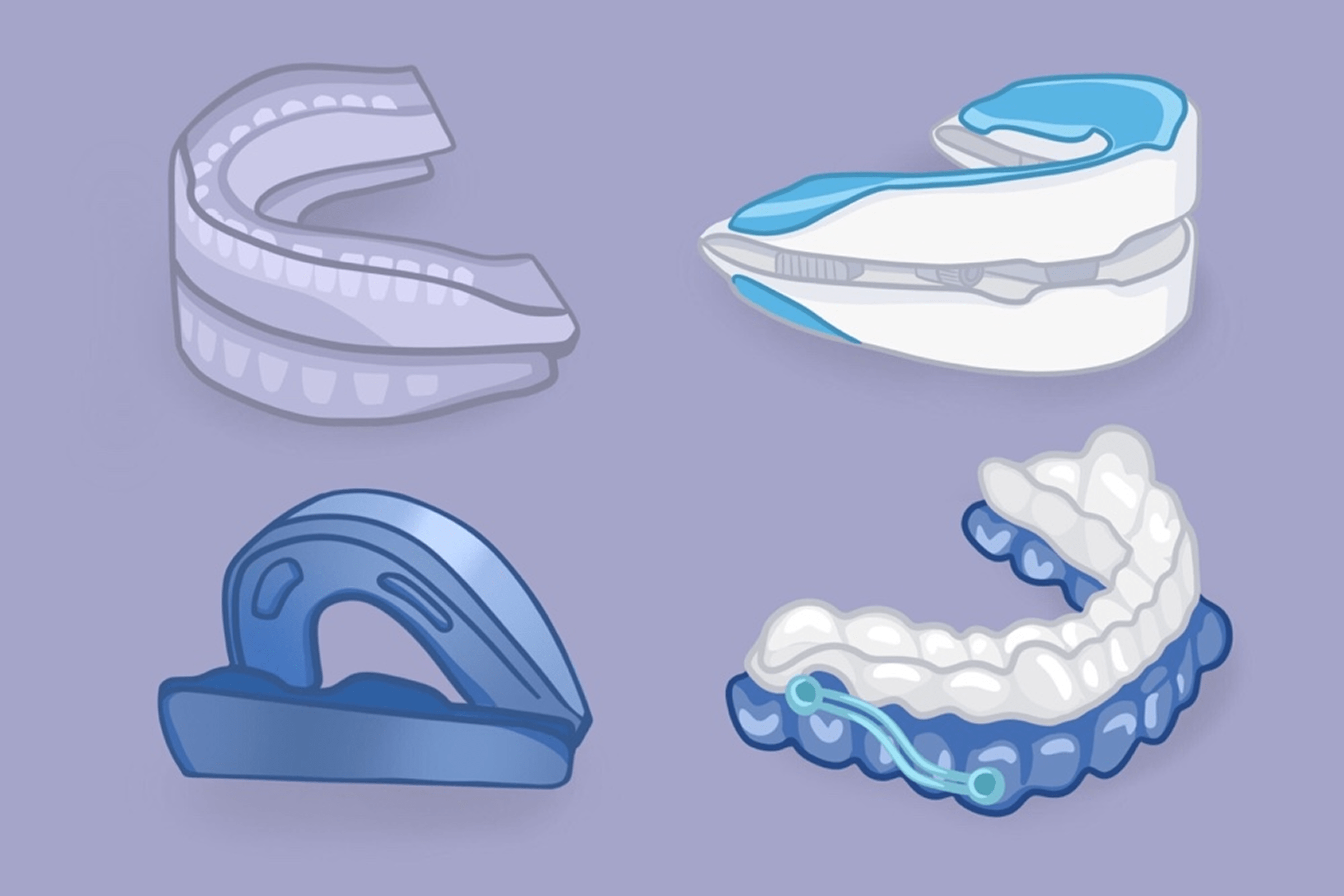
Whilst not recommended for severe cases of OSA, a mandibular advancement device (MAD) can be a good option for those with mild to moderate OSA, or those who do not tolerate CPAP.
MADs brings your lower jaw (mandible) forward (or advance it) to tighten the tissues in your airway that are prone to slackening and causing obstruction.
There are many different types of MAD available so finding the right one can be a bit confusing. To get the best quality we recommend getting a mouthpiece custom fitted by a dentist, though this can be quite expensive.
You can still find great quality mouthpieces without paying loads for a custom-made one. Have a read of our guide to anti-snoring mouthpieces so you know what to look out for when buying generic devices online.
If your tongue causes obstruction in your airway, a different type of mouthpiece called a “tongue retainer” can also be effective for mild to moderate OSA.
CPAP stands for continuous positive airway pressure and is a treatment suitable for moderate to severe sleep apnea sufferers. It is the primary method for managing OSA and has a wealth of evidence to support its efficacy.
In most countries, it is only available with a prescription after confirmed diagnosis of sleep apnea.
A CPAP device uses a mask to force air into your nose and throat to keep your airways open.
CPAP does not give you more oxygen. Instead, it introduces a current of normal air that creates positive pressure; this props open your airway to stop it from collapsing.
Many people are fearful of CPAP. Users can also struggle with their devices, experiencing discomfort, claustrophobia and air leakage.
Despite its scary reputation, it’s important to know that CPAP can be a life-saving tool. There are measures you can take to get the most out of it and cope with any difficulties you may have.
SnoreLab’s guide to dealing with CPAP issues - Check out
.png)
Research has shown that exercising the muscles in your airway can have a positive impact on mild to moderate sleep apnea.
These techniques are adapted from speech and language therapy and consist of repeated movements in the tongue, cheeks, jaw and soft palate in order to increase muscular tone.
Several studies demonstrate that patients with sleep apnea can reduce their AHI scores and sleepiness by performing these exercises regularly [10] [11] [12] [13].
You can read about all of the evidence and also learn the 5 exercises we recommend.
Surgery is usually a last resort only when other techniques to manage your sleep apnea have failed.
Whilst there is some research to show that surgery can produce positive outcomes for OSA, there isn’t enough evidence for surgery to be routinely recommended ahead of alternatives like CPAP.
Usually, to be considered for surgery, there are several requirements that will be assessed by an ENT (ear, nose and throat) specialist first:
There are many types of surgery for snoring and not all are recommended for OSA sufferers.
To get an overview of the surgical interventions available and the important considerations when exploring surgical options, be sure to read our article on surgery for snoring and sleep apnea.
Obstructive sleep apnea can be managed via a number of different means. What is most effective depends on the causes of your condition and its severity.
Regardless of which treatment route you take, many countries have support groups for people with OSA.
These organisations aim to educate and provide support with all facets of OSA.
They give helpful information on living with the condition, provide practical support with CPAP and other treatments, fund and publish the latest research into sleep apnea as well as organising support meetings in person.